HSR News February 2023 | Talking to HSRs, Time to Act on Silicosis
 Talking to HSRs
Talking to HSRs
This month I interviewed some of you about being Health and Safety Reps in your workplaces.
I was interested to hear your stories and experiences, find out the struggles, challenges, wins, and what you think needs to change to make your role more successful.
Each month 1 HSR will be featured, to talk about their experience.
Here is what HSR Dee had to say this month….
Dee, HSR
Dee is coming up to 23 years at her workplace and has been an HSR for 4 years. She has extensive experience and knowledge both within her employment role and as an HSR.
Dee expressed her passion for Health and Safety as she loves to help people, and her role as an HSR has allowed her to do this both in her workplace and on a national level.
As we have heard so many times before, Dee has been a witness to occurrences in the workplace that have not been acceptable and pose a real risk to the safety of workers, and she was kind enough to share a couple of stories with us.
“I was stabbed at work with a pair of scissors (these were stupidly attached to a piece of string that was attached to the leg of a desk). I didn’t see the scissors when I went to pick up a printout and the scissors stabbed me in my leg. If the scissors landed half and inch higher, it would have hit my main artery. I walked 1.5km to my doctor, holding my leg with tissue paper from the toilet, had a tetanus shot and stitches and not a lot of sleep for many nights. I had a couple of sessions of physio some weeks after.”
Dee has also been affected by serious health and safety problems in her family:
“My dad has Asbestosis. There is no cure. He has around 30% lung capacity from this horrible disease. His asbestosis diagnosis is linked to his first workplace at the age of 14 as a Mechanic.”
 In her role as an HSR, Dee has performed many workplace inspections and reported issues.
In her role as an HSR, Dee has performed many workplace inspections and reported issues.
Some of the Health and Safety issues that have been identified/reported to her include:
- COVID 19 issues/concerns
- Broken office equipment
- Lighting issues
- Fumes and noise levels
- Psychosocial hazards including workloads, bullying and harassment.
Dee explained even though they do have what she describes as a ‘fair’ WHS structure in place, they have been shown to not be consistently effective. The main frustration is having blockers to reporting issues/hazards and not having enough HSRs and managers reporting issues due to theses blockers. By “blockers” Dee means, paperwork not getting to the relevant people/unnecessary additional paperwork or, being told that “it is not your job to solve the problem” (if not us then who?). The other frustration is the lack of respect of the rights of an HSR being able to request assistance, including assistance from experts that the HSR has chosen.
Dee said:
“My workplace needs to improve its safety culture. On a personal level, I have a supportive leader who is supporting me in my role as HSR, but this hasn’t always been the case. We could do with more HSRs. Leadership at all levels need to be on the same page about safety and what it practically means in the workplace.
- Actively encouraging staff to speak up about issues and concerns and providing feedback on those concerns, and
- Actively encouraging staff to step into health and safety roles.”
Currently Dee’s workplace has 13 HSRs with 5 HSRs vacant roles, leaving some work groups without a rep. The role of the HSR is recognised at this workplace but Dee believes if the culture was improved then the support to Health and Safety and to the HSRs would be provided.
Finally, we asked Dee what benefits the introduction of the Psychosocial Hazard Code of Practice and Regulation on April 1 would bring to her workplace.
She responded with:
“Workload management and impacts of overload, timing and expectations are of real concern in our workplace. I am hoping that the changes bring a new era of putting worker safety at the forefront of management and decision making. I am hoping that we see real changes in the workplace, that have a positive impact on sustainable workload and output for workers in my workplace.”
Who is at risk of Silicosis?
You are at risk of silicosis if you work with quartz, sand, stone, soil, granite, brick, cement, grout, mortar, bitumen or engineered stone products.
- Making and installing composite (engineered or manufactured) stone countertops.
- Excavation, earth moving and drilling plant operations.
- Clay and stone processing machine operations, paving and surfacing.
- Mining, quarrying, and mineral ore treating processes.
- Tunnelling.
- Construction labouring activities.
- Brick, concrete, or stone cutting; especially using dry methods.
- Abrasive blasting (blasting agent must not contain greater than 1 per cent of crystalline silica).
- Foundry casting.
- Angle grinding, jack hammering and chiseling of concrete or masonry.
- Hydraulic fracturing of gas and oil wells.
- Pottery making.
Not everyone who works with silica dust develops silicosis. The chances of getting silicosis will depend on many factors, including how much silica dust you come into contact with, and for how long you were exposed to it.
Can silicosis be prevented?
Silicosis can be prevented by:
- Avoiding prolonged exposure to silica dust.
- Wearing protective masks (but not disposable paper ones).
- Wetting down tools and materials to suppress dust.
- Using tools that have dust-collecting attachments.
All workplaces, employers and employees in Australia must comply with their workplace health and safety procedures.
For further information on protecting your lungs from silica dust go to the Lung Foundation Australia’s website
Resources and support visit: Safe Work Australia, Lung Foundation Australia, Royal Australasian College of Physicians.
 “Instead of planning a family, we’re planning my funeral.” (Kylie Goodwin – stonemason 7NEWS.com.au)
“Instead of planning a family, we’re planning my funeral.” (Kylie Goodwin – stonemason 7NEWS.com.au)
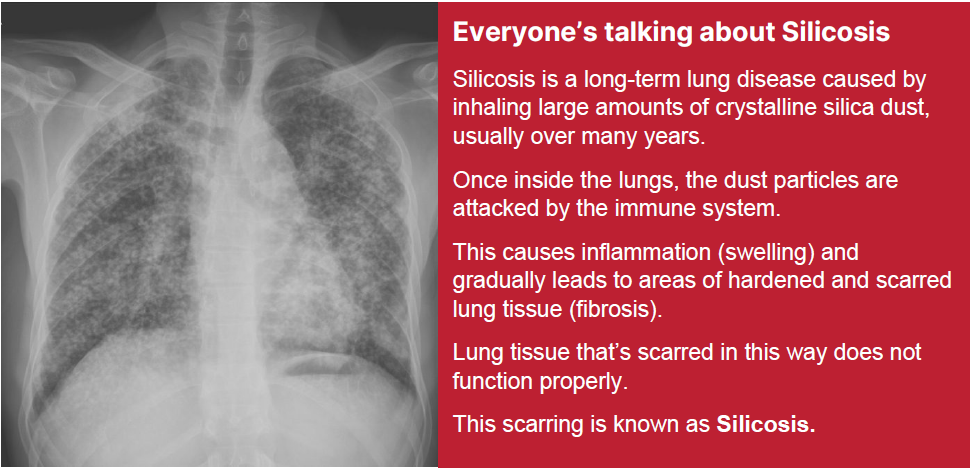
On Tuesday 21st February 2023 7NEWS.com.au posted that Australian tradies and workers are facing a health crisis as new findings reveal the extent of the public health threat silicosis poses to lungs.
Organisations have now called upon regulatory bodies to take immediate action to stop rising cases of silicosis.
The condition is incurable and can cause lung inflammation and fibrosis.
Respiratory Pharmacology Associate Professor Jane Bourke from Monash University said, “silicosis is a devastating occupational lung disease affecting increasing numbers of workers breathing in fine silica dust, causing inflammation and scarring in the lungs”.
“Silica dust particles are 100 times smaller than a grain of sand so can travel deep into the lungs to cause damage. Bourke added, as an example engineered stone used to make kitchen bench tops can contain up to 96% of silica – an amount which is significantly higher than natural stone, - which exposes these workers to unsafe workplaces.”
Silicosis is preventable but is currently incurable, and can lead to other diseases including cancer, and can be fatal.
Those at risk is not restricted to workers working directly with these products. Silicosis has been diagnosed in workers who were working up to 90m away.
 Time for action
Time for action
Organisations and workers are calling for an end to importation and manufacturing of engineered stone in the construction of household kitchens and bathrooms due to the toxic silica dust that it exposes workers to.
Thousands of workers are regularly exposed to the toxic dust during tunneling, and construction companies make it difficult to bring on site dust monitors to regularly monitor workers’ exposure.
There needs to be regular measurements taken of airborne contaminants underground, this includes monitoring with a dust monitor.
The implementation of appropriate PPE and the ability to test levels at a site at any time to establish if unsafe. All dust monitoring results should then be promptly provided to the regulator and the appropriate organisation where there is a vested interest.
Comment made by the ACTU stated, “if we do not act, we will have 100,000 cases of silicosis (and) more than 11,000 with cancer in this country.”
The ‘Lung Foundation Australia’ has called for a public consultation on the Nation Silicosis Prevention Strategy (NSPS) and accompanying National Action Plan (NAP).
If you are at risk in your workplace, take action, get involved to make change and help prevent this disease spreading to more Aussie workers.
[Sources: 7NEWS.com.au, Work Safe Australia, Monash University, ACTU]